Simulation Training Reduced Error Rates in the OR

The publication titled “Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies,” published in the American Journal of Surgery, presents a study that explores the impact of proficiency-based virtual reality training on the error rate of residents during their initial 10 laparoscopic cholecystectomies.
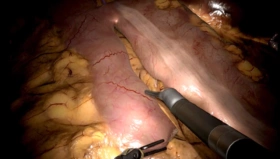
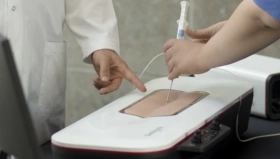
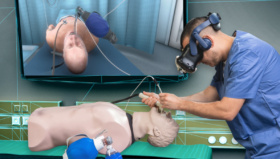
In the study carried out at Karolinska Hospital, Prof Gunnar Ahlberg and his team investigated whether proficiency-based training on the LapSim system improves objectively assessed, intraoperative performance during the initial learning of laparoscopic cholecystectomies (LCs). The researchers divided surgical residents into two groups: one group received proficiency-based virtual reality training, while the other did not receive this specific training. The training program aimed to enhance the residents’ surgical skills and proficiency through simulated virtual scenarios that accurately replicated events and instrument movements in laparoscopic procedures.
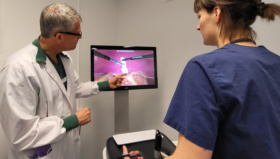
The study yielded noteworthy results, showcasing a substantial reduction in the error rate among residents who underwent virtual reality training. Remarkably, the training group displayed improved performance during their first 10 laparoscopic cholecystectomies on patients compared to the non-training group. This finding underscored the potential educational benefits of virtual reality and was an important milestone for the integration of high-fidelity simulation into surgical trainings that has developed since.
Subjects assigned to the simulation group were allowed to practice for as many 1-hour sessions they needed, during 1 week, to meet proficiency levels as defined by a pool of experts (>300 procedures). All subjects then performed their first 10 individual full procedure LCs under the supervision of an experienced laparoscopic surgeon at each respective center. Surgery number 1, 5, and 10 were blindly assessed from video recordings. Based on a list of 31 defined errors (such as tissue exposure, tissue division and clipping, dissection, etc), video reviewers found that residents in the control group made on average 3 times as many errors as the simulator-trained group.
Notably, the training program followed a proficiency-based approach, tailored to address the individual needs and skill levels of each resident. This personalized approach ensured that residents progressed at their own pace, focusing on areas where additional practice or improvement was necessary: its importance was also reflected in the great variety in number of simulation sessions needed to reach proficiency in the training group, from 161 to 594 attempts.
The study’s findings hold significant implications for surgical education and patient safety. The incorporation of virtual reality training into surgical residency programs has the potential to enhance the overall quality of training and reduce errors during critical surgical procedures.
Moreover, virtual reality training provides a controlled environment where residents can make mistakes without jeopardizing patient safety. These mistakes serve as valuable learning experiences, enabling residents to understand the consequences of their actions and refine their techniques accordingly. By providing a safe space for skill acquisition and error correction, virtual reality training promotes a culture of continuous improvement in surgical education.
Reference: G. Ahlberg et al. / The American Journal of Surgery 193 (2007) 797–804