Mobile COVID-19 Ultrasound Training Unit in France
Dr. Sébastien Mirek set up a mobile unit to support doctors in the use of ultrasound in COVID-19 treatment. The non-invasive, non-irradiating examination can save caregivers time.
The Challenge
Dijon is the capital city of the Côte-d’Or department in the Bourgogne-Franche-Comté region.
During the outbreak of COVID-19 pandemic, the Bourgogne-Franche-Comté region and its surrounding regions were hard-hit with thousands of patients seeking medical care.
Point-of-care lung ultrasound and echo, based on Chinese and Italian experience, was found to be effective for the triage and monitoring of suspected/confirmed COVID-19 patients due to its portability and diagnostic capability for lung and cardiac damage.
Due to the large scale of the outbreak, physicians from various specialties were required to conduct lung ultrasound for the first time as a part of COVID-19 patient care (anesthesiologists, emergency physicians, pulmonologists, pediatricians and more).
The Solution
The USEEM (simulation center of Dijon University Hospital) adapted and strengthened its training in order to support all the professionals who work for the care of patients suspected or detected positive for COVID-19. The training phase is crucial before putting ultrasound into practice, and USEEM has adapted its actions to the coronavirus pandemic.
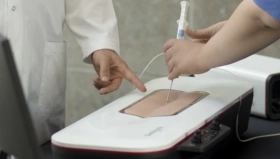
The Simbionix Ultrasound Mentor simulator was used in USEEM for several years, and the center received the new COVID-19 Ultrasound Module as a response to the pandemic. The USEEM was the first center in France to use this innovative module to fight against the pandemic.
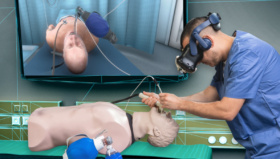
Dr. Mirek, an anesthesiologist-resuscitator at University Hospital Center Dijon-Bourgogne and trainer within USEEM, chose to adapt a system for transportation, and offer training to hospitals outside the CHU Dijon Bourgogne. The mobile training unit only requires two people for transport and using the premises’ ultrasound equipment.

The mobile training unit for COVID-19 is also a French first.
The motto of medical simulation is “never the first time on the patient”, says Dr. Mirek. The U/S Mentor ultrasound simulator with its COVID-19 module is used to teach healthcare professionals to recognize typical ultrasound findings of COVID-19 patient.
“Once we learn the typical findings on the simulator, we can reproduce it on an actual COVID-19 patient,” explains the trainer. Since April 13, 2020, dozens of physicians have been trained on the simulator. “The objective is therefore to train anesthetists, emergency physicians and general practitioners.”
On April 17, the USEEM mobile unit came to offer the Bénigne-Joly mutual health clinic in Talant, on the outskirts of Dijon, COVID-19 ultrasound training on the U/S Mentor simulator given to four anesthesiologist-resuscitators.
A training session begins with disinfecting the simulator before placing the mannequin on a hospital bed. The practitioners follow a training program: videos on the lung ultrasound of a patient with COVID-19 and then hands-on training on the mannequin. The training is either given by a proctor, or an independent training based on the tutorial established by USEEM. The session lasts one hour per trained practitioner.

“The training goal is to be able to use ultrasound to categorize the patients” specifies Dr. Mirek. “We have a patient who has a symptom that resembles COVID-19, the ultrasound allows us to do the triage: normal lung ultrasound, a mild patient with some symptoms; abnormal lung ultrasound, patient with severe course of disease” to determine if the patient requires a transfer to a conventional service or to intensive care unit.
The Outcome
The ultrasound allows patient categorization but not diagnosis per se because the pulmonary lesions identified are not specific to COVID-19. Nevertheless, this provides information to feed a bundle of arguments in order to establish a diagnosis. When patients arrive in large numbers, it is easier to do an ultrasound that takes three minutes rather than a CT scan.
“The advantage of ultrasound is to be non-invasive, atraumatic, non-radiating. It can be done at the patient’s bedside, in the emergency room or even at home,” said Dr Mirek. A next step envisaged is that the general practitioners of SOS Doctors will be able to take images of a patient at home in order to send them to the CHU Dijon Bourgogne for analysis.
Credits for photography: JC Tardivon