Prepare More Confident Surgeons

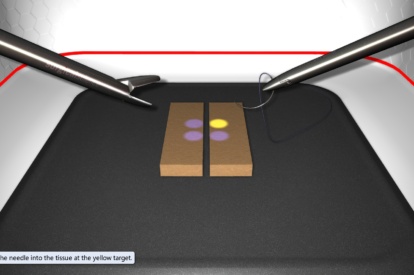
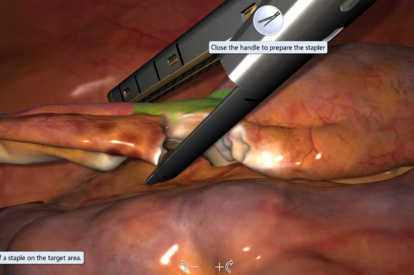
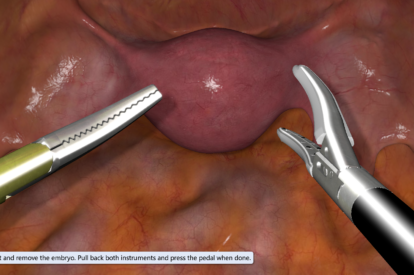
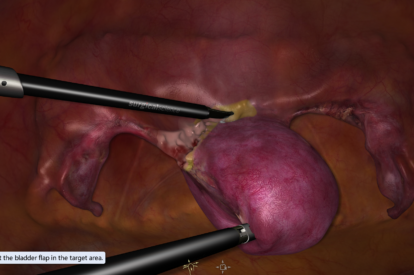
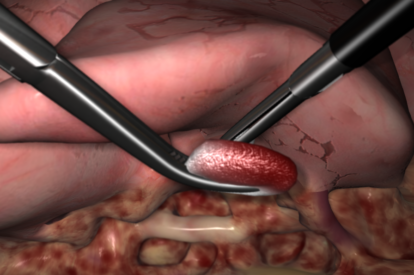
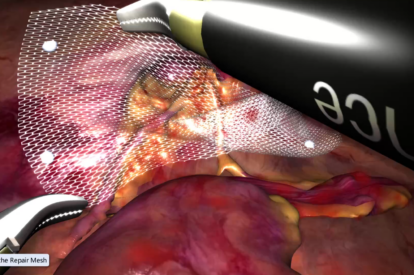
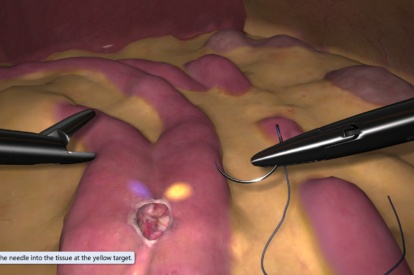
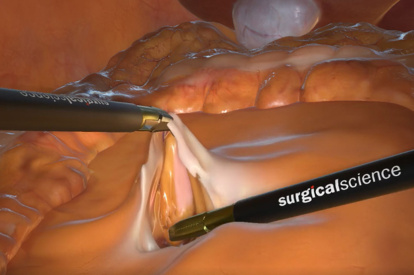
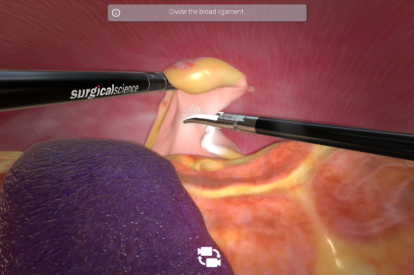
Our pioneering LapSim® simulator can improve your training simply and quickly. Including a range of exercise packages from basic to advanced laparoscopic procedures, it provides residents with an essential path to technical skills proficiency. As a high-fidelity simulator, it gives you tactile feedback, highly realistic and detailed graphics, and a rich immersive training experience.
LapSim comes ready to use: it’s ideal for individual, self-paced training, with its instant performance feedback, and includes an easy-to-use admin mode for course management. Either you customize your own courses and benchmarks to fulfill your own training requirements, or you pick from the pre-set library which includes fully validated curriculums.
LapSim Shortens Time to Surgical Skills
Check out this effective simulator that has proven to reduce medical errors in the OR.

Features and Benefits
- Master psychomotor skills with fundamental and procedural training
- 11 training modules covering abdominal surgery procedures
- Authentic handles with tactile feedback, to develop accurate manual dexterity
- Customizable courses, configurable difficulty levels
- Performance feedback reports, with statistics
- Screen recording for debriefing
- 3D output available
- Instructions available in 8 languages
Testimonials
“VR simulator-trained students perform real surgery with more confidence, less operative time, and increased accuracy. The LapSim Certification Program is definitely a great resource for residency programs…
Dr. Hulda Einarsdottir, MD, FACS, FASCRS
Formerly Assistant Professor of Surgery, Yale University, School of Medicine
"In the last 25 years, I have organized about 50 courses in practical surgery for residents and specialists in Obstetrics and Gynecology. In the courses involving laparoscopy, LapSim has been used to…
Dr Thomas Bossmar, MD, PhD
Consultant at the Women's Clinic and Practicum, SuS in Lund
Validation Studies
Virtual simulator training programme performed at least twice a week was effective for implementing basic surgical skills required for the trainee's professional growth. Additional virtual training modules focused on more complex exercises are planned to confirm these preliminary results.
Impact of virtual reality training on laparoscopic surgery: Residents who trained on Surgical Science LapSim® and followed a predefined curriculum demonstrated a proficiency level equivalent to surgeons who have performed 20-50 patient procedures.
Learn More
Download the LapSim Brochure
Learn more about the LapSim simulator.

Contact Us
Do you want to know more about LapSim?