Surgical Science uses cutting-edge data science to continuously improve its simulation solutions. In an ongoing collaboration, the company has been working with leading urologic surgeon Dr. Andrew Hung and his research team at Cedars Sinai Medical Center on a project to highlight the value proposition of Surgical Science’s new, enhanced simulation data.
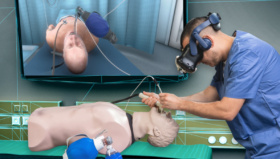
 One of the main benefits of using simulation within medical training is the provision of truly objective and structured assessment data that can ‘score’ trainee performance. Modern Virtual Reality (VR) simulators deliver data insights on user proficiency, ensuring trainees are all reaching the required standards and allowing educators to coordinate training programs more effectively.
One of the main benefits of using simulation within medical training is the provision of truly objective and structured assessment data that can ‘score’ trainee performance. Modern Virtual Reality (VR) simulators deliver data insights on user proficiency, ensuring trainees are all reaching the required standards and allowing educators to coordinate training programs more effectively.
For years, Surgical Science has led the way in the use of data science in simulation, and it is continuously working on delivering higher levels of granularity within its data output. While VR simulators have always been able to produce basic metrics and scores, the team is using artificial intelligence to go deeper into the kinematics of a simulator’s instruments and ‘learn’ how fine motor skills and techniques are performed by surgeons.
It is vital that this kind of innovation is validated in a clinical setting, so Surgical Science works with research groups to quality test its new simulation technology.
Renowned urologist Dr. Andrew Hung of Cedars Sinai Medical Center (Los Angeles, California) has put together a team of clinicians, engineers and scientists to carry out groundbreaking research on the use of simulation during the training of RARP (robot assisted radical prostatectomy) procedures.
 Dr. Hung and his team incorporated Surgical Science’s FlexVR simulation platform in their NIH-funded (National Institutes of Health) five-year long research study ‘Deep Stitch’ – which set out to compare suturing assessment scores attained by surgeons using VR simulators with manually assessed analysis of the same surgeons performing in a live RARP case.
Dr. Hung and his team incorporated Surgical Science’s FlexVR simulation platform in their NIH-funded (National Institutes of Health) five-year long research study ‘Deep Stitch’ – which set out to compare suturing assessment scores attained by surgeons using VR simulators with manually assessed analysis of the same surgeons performing in a live RARP case.
“We wanted to see if virtual reality simulation-based assessment of suturing skills can be used as a proxy for a surgeon’s ‘live’ suturing skills,” says Dr Hung. “If we could prove there is correlation in the data, we could use these computer-generated metrics to provide valuable insight into suturing technique, and translate it into direct, actionable feedback.”
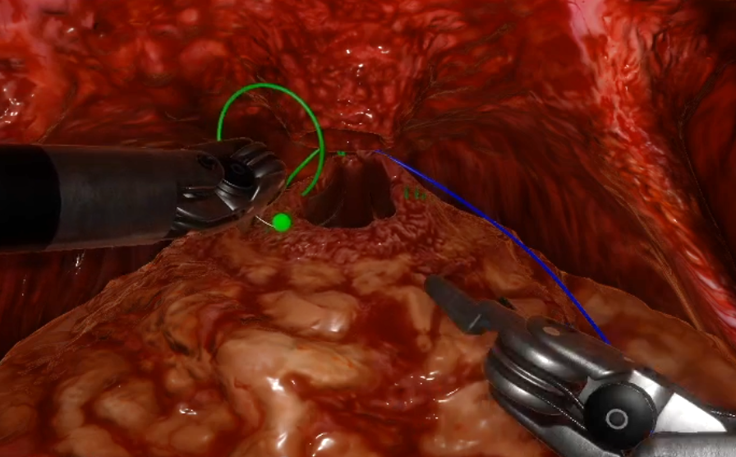 More than 40 urologists took part in the research, from trainees to highly experienced practitioners. They performed anastomosis suturing skills (an important step in the RARP procedure), first on the simulator and then in the operating room, where the surgeries were filmed and analyzed using a validated assessment rubric, End-To-End Assessment of Suturing Expertise (EASE) 1.
More than 40 urologists took part in the research, from trainees to highly experienced practitioners. They performed anastomosis suturing skills (an important step in the RARP procedure), first on the simulator and then in the operating room, where the surgeries were filmed and analyzed using a validated assessment rubric, End-To-End Assessment of Suturing Expertise (EASE) 1.
This study went a step further than usual in that it collected patient-reported outcomes for these RARP cases to study the relationship between EASE assessment within VR simulation and patient outcomes – which is the holy grail for this type of research. “Showing VR data metrics can approximate OR performance is great, but we are excited about the initial results showing data insights from simulation are associated with patient outcomes!” says Dr. Andrew Hung.
The results showed high levels of correlation in the data gathered using both methods, proving that the simulators can successfully capture a surgeon’s suturing performance in a holistic manner. More importantly, it showed that there is a strong association between assessment in VR simulation and key patient outcomes like 3-month continence.
“The research proved that our simulation technology is capable of providing higher levels of detail and an accurate capture of surgical technique than ever before,” says Anand Malpani, Director of Data Science in R&D at Surgical Science. “We go beyond the usual metrics delivered by many simulation tools and deliver insights that are hard to obtain from observing live surgeries due to the complexities involved in analyzing surgical videos.”
The collaboration is proving mutually beneficial. For the R&D team at Surgical Science, the research is delivering clinical proof-of-concept, allowing them to move forward with next-generation software for the company’s new suite of data-powered simulation training solutions. For Dr. Hung and his team, the Surgical Science simulators are providing levels of data granularity that have not been available before, helping them reach the ultimate goal of proving that simulation can deliver insights about critical real-world safety and quality metrics like patient-reported outcomes.
Dr. Hung’s initial conclusions found that, as well as proving the ‘transferability of skill assessments between VR simulation and live surgery’, there was ‘a positive association between ideal scores for VR needle hold angle and driving smoothness subskills and 3-month continence recovery.’
“This is the next generation of simulation technology,” Anand says. “Through partnerships with research groups like Dr. Hung’s, we are gathering the clinical evidence we need to bring new data insights to the market. Our simulators will be able to predict the OR readiness of a trainee based on such insights that are built on top of such clinical AI research. This particular study was concentrated on urology, and specifically anastomosis in RARP procedures, but we are confident that it also applies across all healthcare scenarios and shows that simulation is helping to power the digital evolution of the patient’s surgical care pathway right through the operating room.”
Surgical Science and Dr. Hung’s partnership continues to explore the frontiers of data-driven simulation training and its relation to real world patient outcomes. Dr. Hung’s next NIH-funded research project “Deep Dissect” is already underway looking into the neurovascular bundle dissection in RARP procedures. Dr. Hung’s team has shown promising results 2 in leveraging this next generation of simulation data from Surgical Science to train AI algorithms that can automatically analyze performances from the OR. Stay tuned for more on these exciting projects using Surgical Science simulation technology.