Interview with Lars Konge, the head of research at CAMES (Copenhagen Academy for Medical Education and Simulation) a world leading academy for medical education and simulation.
Why do you think it’s been so slow for other countries to take up VR simulation training? Do people like to hold on to traditional methods?
We need more solid research showing that you can save money with VR simulation. And a political system that allows the money that you save in the hospital to be transferred to the training centers. Every time we save a complication, we should get that money back to our center. I think that Denmark is starting to see the bigger view of this. And our regional government has transferred money over to us in the past years.
Yes, it’s a lot of short-term thinking. That’s how politics works.
It’s crazy the amount of money spent on reoperations and the indirect hospital costs. If we can reduce the reoperation rate by 1%, then the amount of money we save, will be able to drive a complete training program in Denmark for more than 10 years. It’s almost embarrassing that you need to make these calculations because just from an ethical viewpoint training on patients shouldn’t be happening.
There doesn’t seem to be much public awareness about how much training is done on patients.
It’s mad because nobody really wants to know. Perhaps only simulator companies. The politicians want to say that we have a 100% safe and superior healthcare system. Doctors like myself want to be part of that tale – and the patients want to believe it.
A publication from 1999, estimated that 98,000 Americans died every year of medical errors that could have been prevented. And in 2015, the British Medical Journal published a study from John Hopkins saying that that number was probably closer to 250,000 – making medical errors that could have been prevented, the third largest cause of death in the US. Simulation could help solve a lot of these problems.
Do you think there are other reasons why VR simulation has become a more established tool?
I see another drive. There’s been a cultural change in the trainees as well. They enjoy the training, but they find it unethical to perform on a patient for the first time. Young doctors find it weird when a supervisor allows them to do an operation that you have not been trained for in the SIM center. And that’s been a long journey that has taken 10-15 years.
This is a new generation of doctors, they are going to drive the change. I am probably one of the last of the old generation. My colleague recently said that he had a trainee, who was going to do his first bronchoscopy but first we will send him to the SIM center because he was not feeling comfortable. That would be unheard of 10 years ago.
This is what I hear most, how trainees feel more comfortable and have more confidence in the OR, once they have used a VR simulator.
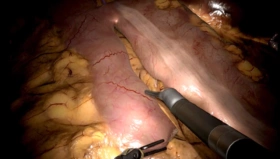
Yeah, and now we have all these the metrics on, for instance, laparoscopy simulators. The metrics have really improved over the years and the number of validation studies helping us to find the right metrics. This allows us not only to do tests but to also to use these metrics as feedback.
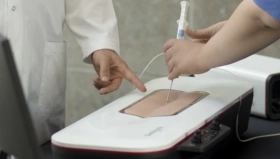
We have published a paper showing that automated feedback from the simulator makes you practice harder, longer, and in a smarter way. Normally you see trainees just doing basic tasks, two or three times, and then they want to do the real stuff and they become cognitively overloaded and stop practicing because it’s too difficult.
So instead, we build them up using the metrics in the simulators. We can do this using medical students as assistants rather than experienced supervisors and allowing the trainees to make mistakes. That’s another important part of simulators, if you don’t make mistakes, you don’t improve. Obviously, I would never argue for that kind of training in the real environment.
You can also increase the difficulty, add challenges, change camera angles with a simulator.
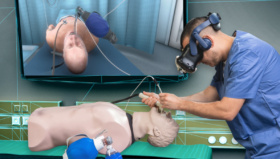
Yes. We’ve even taken that further now and started to create VR full immersion scenarios, where you take the VR simulator into a full VR environment and it showed that they learned less when they had the full immersion experience.
When we investigated the data, it was due to cognitive overload. They were so overloaded by having to react to the nurses, anesthesiologists, and the entire environment that they couldn’t focus on learning.
That’s a good example of how it is to learn on patients, where they’ve got so much going on around them, in a stressful environment.
Yes, that’s correct. There is scientific proof that it’s not a good learning environment to be in a stressful situation.
And, robotic surgical training? You’ve started this traning at CAMES?
I’m happy that you asked that. Last week we got our funding to be the regional mandatory training center. Training in VR simulators, live pigs and team-based training.
So now, it’s mandatory. If you want to become a robotic surgeon, you will need to go through our program. We have two PhD students working in this area and I think that the future is where we see a lot more simulator companies supporting robotic companies, that have had a monopoly for many years now. It’s good to have competition, especially in training, because the training has been run by the company. I believe that we should not let companies train our doctors, it should be the hospitals or the simulation centers.
Yes, exactly. Is this something that you think is evolving in other med schools and universities around the world. Are they taking on robotic surgery training?
Yes, but it’s postgraduate trainings or it’ll be in post-graduate simulation centers. When you are still in med school, you’re far away from doing robotics.
A new product, like a robotic system does not have any value to hospitals and patients without trained surgeons. And luckily all robot companies have realized that, so the emerging robotic companies want to have structured training. At CAMES we are working very closely with several of these companies.
And you’ll be writing papers about the benefits of this type of robotic training.
Definitely. We are striving to get as far up on the Kirkpatrick Pyramid as possible, no longer just saying that that trainees liked to practice on a simulator but proving that patients do better. And with simulation-based training, it’s cheaper to practice on a simulator than on a patient.